 English
EnglishDangerous complications of diabetes and the role of nutrition in prevention strategies
Diabetes complications are a major health burden, but they are completely preventable if patients are fully equipped with scientific knowledge and effectively apply disease control measures. This article, from a professional perspective, will clearly analyze the most dangerous risks: from retinopathy, kidney disease to myocardial infarction and stroke. The focus of the article is on preventive solutions, especially the role of nutrition in controlling blood sugar and cardiovascular risk factors.
Why are complications of diabetes dangerous?

Diabetes causes many dangerous health complications
Diabetes is not simply a disease of high blood sugar. Its real danger lies in the silent but devastating damage that chronic hyperglycemia causes throughout the body. The basis of all diabetic complications originates from a common mechanism: damage to the endothelium.
The endothelium is a fragile lining inside all blood vessels, from the tiny capillaries in the eyes, kidneys, and nerves, to the large arteries that nourish the heart and brain. When blood glucose levels are high for a long time, it causes a complex series of biochemical reactions, including oxidative stress, production of advanced glycation end products (AGEs), and activation of inflammatory pathways. All of these factors attack and damage the endothelium, causing blood vessels to become stiff, less elastic, more susceptible to inflammation, and to form atherosclerotic plaques.
Depending on the location and size of the damaged blood vessels, complications manifest in different organs. Understanding them is the first and most important step to building an effective prevention strategy.
Small blood vessel (microvascular) complications
These are typical complications of diabetes, occurring in blood vessels with very small diameters.
Eye damage (diabetic retinopathy): Leading risk of blindness
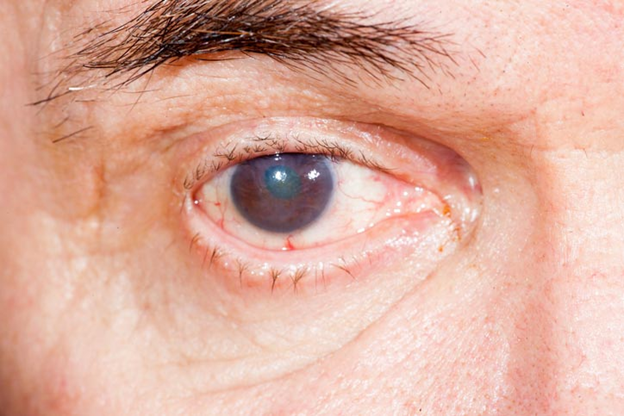
Diabetic retinopathy
The retina is a light-sensitive layer of nerve tissue at the back of the eye, nourished by a dense network of blood vessels. Chronic high blood sugar causes these blood vessels to weaken, become microaneurysms, and begin to leak fluid or blood into the retina, causing macular edema. This is the main cause of vision loss in the early stages. As the disease progresses (proliferative stage), the body responds by creating new, fragile blood vessels. These blood vessels can cause severe bleeding in the eye, scar tissue formation, and eventually lead to retinal detachment, causing permanent vision loss. Diabetic retinopathy is now the leading cause of blindness in working-age adults in developed countries.
Kidney damage (diabetic nephropathy): Leads to end-stage renal failure
Each kidney contains millions of tiny blood-filtering units called glomeruli. The microscopic blood vessels in the glomeruli filter waste from the blood to form urine, while retaining important substances such as protein. High blood sugar and high blood pressure (which often accompany diabetes) damage these microvessels, causing them to “leak”. The earliest sign of kidney damage due to diabetes is the appearance of small amounts of protein (microalbumin) in the urine. Over time, the damage becomes more severe, leading to a gradual decline in the kidney’s filtering ability. The danger is that the disease often progresses silently, without obvious symptoms until most of the kidney function is lost. If not treated promptly, the disease will progress to end-stage chronic kidney failure, forcing the patient to depend on kidney replacement treatments such as dialysis or kidney transplantation.
Nerve damage (diabetic neuropathy): Pain and loss of sensation
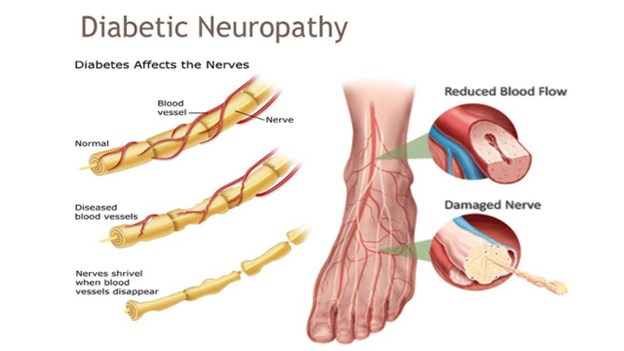
Diabetic neuropathy
Nerves in the body are also nourished by micro-vessels. High blood sugar damages these blood vessels, leading to a lack of blood and nutrients to the nerve fibers, causing diabetic neuropathy. The most common form is peripheral neuropathy, which mainly affects the longest nerves, which go to the feet and hands.
Symptoms of nerve damage in diabetes are very diverse: from burning, prickling or crawling pain, to numbness and, most dangerously, loss of sensation. The loss of protective sensation makes it impossible for the patient to recognize small wounds, calluses or sharp objects piercing the feet. These injuries are easily overlooked, progressing to deep ulcers, severe infections and the risk of gangrene, forcing amputation.
Macrovascular (large vessel) complications: Life-threatening events
Hyperglycemia not only destroys microvessels but also accelerates atherosclerosis in large arteries leading to serious cardiovascular events.
Cardiovascular disease: Myocardial infarction and heart failure

Cardiovascular complications are common in people with diabetes
Diabetes is considered a risk factor equivalent to coronary artery disease. It strongly promotes the process of atherosclerosis, causing cholesterol plaques to accumulate in the coronary arteries that feed the heart and narrow the lumen. When an atherosclerotic plaque ruptures, a blood clot will form at that location, completely blocking blood flow to an area of the heart muscle and leading to an acute myocardial infarction.
A dangerous feature of diabetic patients is that they may have “silent myocardial ischemia” or have atypical chest pain symptoms due to sensory nerve damage. This delays the diagnosis of complications and emergency treatment. Furthermore, diabetes also directly damages the heart muscle, leading to heart failure and causing the heart to not be able to pump enough blood to nourish the body.
Cerebrovascular disease: Stroke (cerebrovascular accident)
The mechanism of stroke in diabetic patients is similar to that in the heart. Atherosclerosis narrows the carotid arteries and arteries in the brain. A plaque can grow large enough to block a blood vessel in place, or a part of the plaque can break off and form a blood clot that travels to the brain, blocking a smaller blood vessel in the brain. Both cases lead to ischemic stroke, causing a region of the brain to die due to lack of oxygen and nutrients. Diabetic patients are 2-4 times more likely to have a stroke than people without the disease.
Nutrition – the most important foundation for controlling blood sugar and preventing complications
Strict control of blood sugar, blood pressure and blood lipids can significantly reduce the risk and slow the progression of the above dangerous complications. In particular, nutrition plays a core role that patients can actively control every day.
Principle 1: Smart carbohydrate control – the golden key to stabilizing blood sugar
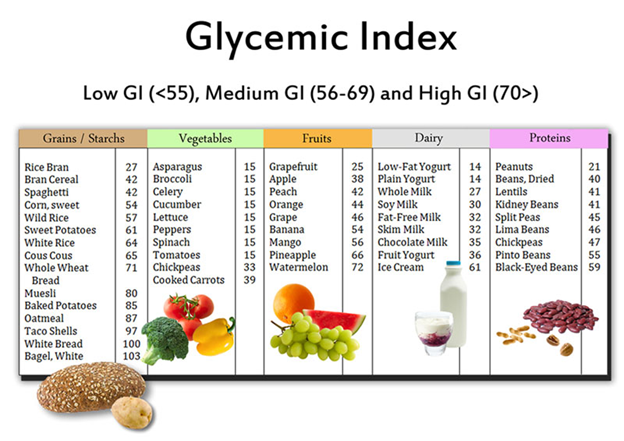
Choosing foods with a medium or low GI for people with diabetes
Of the three groups of energy-producing substances including carbohydrates, proteins and lipids, carbohydrates (carbs) are the substances that have the most direct and powerful influence on blood sugar levels after meals. Therefore, carb management is the most important nutritional strategy for people with diabetes.
To effectively manage carbs in the daily diet, patients need to pay attention to the following 3 important points:
- Choose the right type: Prioritize complex carbs, which have a low to medium glycemic index (GI). These foods are high in fiber, which is digested and absorbed slowly, allowing blood sugar to rise slowly and steadily. Good choices include: brown rice, whole grain oats, quinoa, sweet potatoes, beans (black beans, chickpeas, lentils).
- Minimize: Simple and refined carbs asthey often have a high GI. These carbs are absorbed almost immediately and cause a spike in blood sugar. Therefore, in the patient’s diet, they should avoid foods such as: sugar, candy, soft drinks, honey, white bread, white rice, vermicelli, pho or regular noodles.
- Portion control: Even when choosing good carbs, diabetics still need to eat them in moderation. And to control carbs, diabetics can apply the “plate method” as a simple and effective management method. Diabetics need to divide their plate into 4 parts, in which 1/2 of the plate is non-starchy vegetables, 1/4 is lean protein, and the last 1/4 is for carb-containing foods.
Principle 2: The power of fiber – the “gatekeeper” that slows down sugar absorption
Fiber, especially soluble fiber, has the ability to absorb water and form a thick gel layer in the intestine. This gel layer acts as a “barrier” to slow down the process of emptying the stomach and the process of absorbing sugar from the intestine into the blood. As a result, the post-meal blood sugar peak will be lower and come later. In addition, insoluble fiber increases stool volume, promotes intestinal motility and maintains digestive health.
Therefore, in the daily diet, people with diabetes need to increase the variety of green vegetables such as broccoli, spinach, cabbage and low-sugar berries such as strawberries, blueberries, beans, nuts and whole grains. The recommended goal is to consume about 14g of fiber for every 1000 calories, equivalent to about 25-38g of fiber per day.
Principle 3: Choose healthy proteins and fats – build muscle and protect the heart

Choosing good proteins and fats enables stabilization of blood sugar in people with diabetes
Protein increases satiety, slows the absorption of meals, and stabilizes blood sugar. Healthy fats, especially monounsaturated and polyunsaturated fats, play an important role in reducing inflammation, improving insulin sensitivity, and protecting heart health – one of the most important goals in diabetes management.
Therefore, some advice on choosing foods rich in protein and good fats for people with diabetes is as follows:
- Lean protein: Prioritize fish (especially fatty fish), skinless poultry, eggs, tofu, soy products.
- Good fats: Increase Omega-3 from salmon, herring, sardines and use monounsaturated fats from extra virgin olive oil, avocado or nuts (almonds, walnuts).
- Avoid: Saturated fats found in animal fats, poultry skin, deep-fried foods and absolutely avoid trans fats commonly found in industrial biscuits, fast food or stick margarine.
Principle 4: Pay attention to salt and sodium – reduce the burden on the kidneys and blood pressure
High blood pressure is a dangerous complication of diabetes. A diet high in salt (sodium) is the leading cause of high blood pressure, putting additional pressure on the blood vessel walls, heart, and especially the fragile microvessels in the kidneys, as well as accelerating the progression to kidney failure.
Therefore, diabetics should pay special attention to limiting sodium consumption to less than 2,300 mg/day (equivalent to one teaspoon of salt). At the same time, patients need to form the habit of reading food labels as well as minimizing processed foods, canned foods, fish sauces and pickles. Do not forget to practice the habit of lightly seasoning, using natural herbs and spices to enhance the flavor of dishes is also a useful advice for diabetics.
For many patients, strict adherence to an ideal diet can be challenging. In these cases, specialized Medical Nutrition solutions serve as an important support tool, allowing to fill nutritional gaps and manage the disease more effectively.
Researched and developed by Nutricare and the Nutricare Medical Nutrition Institute – USA (NMNI-USA), Glucare Gold is a scientific nutritional solution that meets the nutritional needs of people with diabetes. The slow-absorbing carbohydrate system in Glucare Gold supports blood sugar balance, and has been clinically proven to have a low GI index for people with diabetes, as recommended by the World Health Organization (WHO).
The product provides Omega 3,6,9 fats and Antioxidants to reduce cardiovascular complications and prevent stroke. The formula supplements 56 nutrients including vegetable protein and whey protein from the US to help compensate for nutritional deficiencies, enhance resistance and support health recovery, reducing the feeling of fatigue often found in patients. In addition, Glucare Gold also supplements Lactium, which has been clinically proven to enhance good sleep, along with soluble fiber FOS to support a healthy digestive system. Glucare Gold is the right nutritional choice, supporting diabetics to stabilize blood sugar, improve health and live with peace of mind.
3 important factors that is indispensable for living well with diabetes

Physical activity improves the health of people with diabetes
Nutrition is an important foundation, however, to build a solid “fortress” against complications, diabetics need a combination of the following 3 factors:
- Regular physical exercise: Exercise helps muscle cells use glucose more efficiently, thereby increasing the body’s sensitivity to insulin. The exercise goal for people with diabetes is at least 150 minutes of moderate-intensity exercise (such as brisk walking or cycling) per week, divided into at least 3 days a week.
- Comply with doctor’s treatment: Diabetes medication is an indispensable tool to bring blood sugar to the target. Taking medication on time, in the right dose, and not stopping medication on your own is extremely important.
- Regular health check-ups and screening for complications: “”Early detection, early intervention” is the golden key in managing the patient’s health. Therefore, it is necessary to follow a regular check-up schedule so that the doctor can check the HbA1c index, blood pressure, blood lipids and perform more in-depth screenings such as funduscopy, microalbuminuria test or foot examination to detect the earliest signs of damage.
Conclusion
Dangerous complications of diabetes are not inevitable in patients. They are the result of damage caused by high blood sugar, and can be completely prevented or slowed down by controlling blood sugar, blood pressure and blood lipids well. Of which, nutrition is the strongest foundation that you can actively control every day. This foundation is built from balanced meals, rich in fiber and healthy fats. This is not only a smart choice but also a direct mechanism to help stabilize blood sugar, while protecting important organs such as the heart, kidneys and eyes.
Nutrition helps prevent complications of diabetes
Therefore, turning knowledge into action: combining a scientific diet, regular exercise and strictly following the doctor’s regimen is the guiding principle in health management for diabetics. You absolutely have enough power to control and write a positive health story for yourself.
References:
|
