 English
EnglishNutrition for rheumatoid arthritis: Foods to reduce inflammation and improve symptoms
According to statistics from the Vietnam Rheumatology Association, the rate of people with rheumatoid arthritis in our country accounts for about 0.5% of the adult population. This number, combined with the trend of the disease getting younger, shows an alarming situation.

What are recommended food for people with rheumatoid arthritis?
In that context, the role of nutrition in a multimodal treatment regimen becomes more important than ever. This article provides you with advice on what to eat, from the golden foods rich in anti-inflammatory Omega-3, to the trio of Calcium, Vitamin D3 & K2 to protect bones and which foods to absolutely avoid. At the same time, the content of the article also points out the “enemies” that cause inflammation such as sugar, bad fats, and processed foods. Applying scientific knowledge to your daily diet is an effective tool, actively supporting pain management, protecting bone and joint function, and improving overall health.
The role of nutrition in rheumatoid arthritis treatment

Diet is extremely important for people with rheumatoid arthritis
Rheumatoid Arthritis (RA) is a chronic autoimmune disease characterized by the body’s immune system mistakenly attacking its own tissues, primarily the synovial membranes of the joints. This attack causes a persistent inflammatory response, leading to swelling, pain, stiffness, and over time can destroy articular cartilage and underlying bone, causing joint deformity and disability.
In the RA treatment regimen, medication is an irreplaceable factor in controlling disease activity. However, in addition to medication, nutrition also plays an extremely important and indispensable supporting role. A scientifically constructed diet can bring multi-dimensional benefits, directly affecting the pathophysiology and quality of life of the patient:
- Reduce systemic inflammation: Food components can regulate the production of cytokines – inflammatory messenger molecules such as TNF-α, Interleukin-1 (IL-1), and Interleukin-6 (IL-6). By choosing anti-inflammatory foods and limiting inflammatory foods, we can reduce the “fuel” for the smoldering inflammation in the body.
- Pain and stiffness reduction: The level of pain and stiffness is often proportional to the level of inflammation. When inflammation is better controlled, swelling and edema in the joint will decrease, thereby releasing pressure on sensory nerve endings and improving clinical symptoms.
- Supports maintaining ideal weight: Being overweight or obese puts a huge mechanical burden on weight-bearing joints such as the knees, hips or spine, aggravating pain and accelerating joint damage. In addition, adipose tissue is also an active endocrine organ, capable of producing inflammatory substances, creating a vicious cycle of disease. Maintaining a reasonable weight through nutrition is a solid foundation intervention to reduce joint pain.
- Improve overall health and energy: People with rheumatoid arthritis are at increased risk for co-morbidities such as cardiovascular disease, osteoporosis, and chronic fatigue. A healthy diet helps protect the heart, strengthen bones, and provide steady energy, giving people the strength to face the challenges of the disease.
Essential nutrients reduces inflammation and protects bone and joint health
To achieve these goals, it is important to focus on specific nutrient groups that have been scientifically proven to have a positive impact on rheumatoid arthritis.
Omega-3 fatty acids: Powerful anti-inflammatory “Weapons”

Omega 3 – Effective anti-inflammatory weapon
Omega-3 fatty acids, especially eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are considered to be among the most effective anti-inflammatory nutrients. The anti-inflammatory mechanisms of these two fatty acids are as follows:
- Competition and substitution: There is always competition between Omega-3 and Omega-6 fatty acids in the body, and consuming too much Omega-6 compared to Omega-3 can lead to inflammation. Specifically, Omega-6 fatty acids, especially Arachidonic Acid, when metabolized can produce inflammatory eicosanoids (such as prostaglandin E2, leukotriene B4). In contrast, Omega-3 can counteract these effects and reduce inflammation. Experts recommend maintaining the best Omega-3 and Omega-6 ratio of 1:1 to 4:1 to optimize health benefits and reduce the risk of inflammation. In contrast, when EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are metabolized, they can produce eicosanoids, but not all of them cause inflammation. Some eicosanoids produced from EPA and DHA have anti-inflammatory properties.
- Production of anti-inflammatory substances: EPA and DHA are precursors for the body to synthesize a special group of compounds called “Specialized Pro-resolving Mediators” (SPMs), including resolvin, protectin and maresin. Unlike anti-inflammatory drugs that simply inhibit, these SPMs actively “quench” the inflammatory response, clean up cellular debris and bring tissues back to a state of balance. This is a natural and effective anti-inflammatory mechanism of the body.
Thanks to these two specific mechanisms, omega 3 has become the first “weapon” in nutrition to support inflammation. The most abundant food sources of omega 3 are cold-water fatty fish such as salmon, mackerel, herring, sardines and anchovies. Plant sources such as walnuts, flaxseeds, chia seeds provide another form of Omega-3, ALA, but the body’s ability to convert ALA into EPA and DHA is quite limited.
Calcium: The foundation for strong bones, preventing osteoporosis
Patients with rheumatoid arthritis face a significantly higher risk of osteoporosis than the general population. This is because chronic inflammation itself produces inflammatory cytokines that stimulate the activity of osteoclasts. At the same time, the long-term use of corticosteroids causes common side effects such as reduced calcium absorption and increased calcium excretion through the kidneys. Calcium is the main structural component of bone, accounting for up to 99% of the calcium in the body. Therefore, ensuring adequate daily calcium intake is a basic and mandatory step to maintain bone mineral density, slow bone loss and reduce the risk of osteoporosis-related fractures.
In foods, milk and low-fat dairy products (yogurt, cheese) are rich and easily absorbed sources of calcium. Other sources of calcium include sardines or salmon with the bones, dark green leafy vegetables low in oxalates (collard greens, kale, broccoli), and tofu.
Vitamin D3: Calcium “transporter” and immune regulator

Vitamin D3 allows transport of calcium into bones
Vitamin D3 is not only a vitamin but also acts as a hormone with two key roles for rheumatoid arthritis patients:
- Calcium Absorption: Vitamin D3 plays a crucial role in supporting the intestines absorb calcium from food into the blood. It stimulates the synthesis of the protein calbindin-D, a protein that transports calcium through the intestinal wall. Without enough Vitamin D3, no matter how much calcium we supplement, most of it will be excreted, making supplementation less effective.
- Immune regulation: This is a particularly important role in autoimmune diseases. Key immune cells such as T cells, B cells, and antigen-presenting cells all have receptors for Vitamin D3. When vitamin D3 binds to these receptors, it can regulate the immune response, reducing the activity of inflammatory T cells (Th1, Th17) and enhancing the activity of regulatory T cells (Tregs) that function to “suppress” the immune system, to prevent autoimmune attacks.
In nature, the main and most effective source of vitamin D3 supplementation is from the synthesis of the skin under the influence of UVB rays in sunlight. However, indoor lifestyle, use of sunscreen and geographical factors cause many people to be deficient. Only few natural foods contain a large amount of vitamin D3, mainly fatty fish, egg yolks and products fortified with vitamin D3 (milk, cereals). Therefore, testing the concentration of vitamin D3 in the blood and supplementing as prescribed by a doctor is very common and necessary.
Vitamin K2: The smart “guide” for calcium
If vitamin D3 is responsible for transporting calcium from the intestines into the blood, vitamin K2 acts as a smart “guide” to ensure that calcium is transported to the right destination. Vitamin K2 activates two important proteins:
- Osteocalcin: This protein, after being activated by vitamin K2, is able to “attach” calcium to the crystal lattice of bones, enabling effective bone mineralization process.
- Matrix Gla-Protein (MGP): This protein is found in soft tissues, especially blood vessel walls. When activated by vitamin K2, MGP becomes a powerful inhibitor of calcification, preventing calcium from depositing in unwanted places such as vessel walls. This is extremely important as rheumatoid arthritis patients are at higher risk of cardiovascular disease, and preventing arterial calcification is an important health goal.
Natural sources of vitamin K2 typically come from natto, a Japanese fermented soybean dish. It is considered the richest source of vitamin K2 (MK-7 form). Other sources include hard cheese, soft cheese, egg yolks, liver, and meats.
Identifying the “enemies” that cause inflammation: Foods to avoid or cut down on
In addition to supplementing beneficial nutrients, identifying and limiting food groups that can promote inflammation is also an indispensable part of a nutritional strategy.
Refined sugar and starch

Refined sugar and starch increase inflammation
Consuming simple sugars and refined starches that have had their fiber removed causes a sharp increase in blood sugar levels. In response, the pancreas releases large amounts of insulin. High insulin levels and fluctuations in blood sugar have been shown to stimulate the body to produce inflammatory cytokines. Furthermore, excess sugar in the blood can react with proteins or fats to create “advanced glycation end-products” (AGEs). These are compounds that are potent promoters of inflammation and oxidative stress.
Therefore, people with rheumatoid arthritis should especially avoid foods containing simple sugars and refined starches such as: soft drinks, candies, tea, white bread, white rice, regular noodles and sugary breakfast cereals.
Saturated fat and trans fat
Saturated fats, when consumed in excess, can activate receptors on the surface of immune cells such as Toll-like receptor 4 and initiate a cascade of inflammatory signaling. Trans fats, often created during the hydrogenation of industrial vegetable oils. The body does not recognize this “foreign” chemical structure, leading to systemic inflammation. They also increase bad cholesterol (LDL) and decrease good cholesterol (HDL).
Saturated fats and trans fats are commonly found in deep-fried foods (such as fried chicken, French fries), fast foods, commercial crackers, margarine, animal fats, poultry skin, and products labeled “partially hydrogenated oil” on the label.
Red meat and processed foods

Red meat and processed meat increase inflammation
Red meats such as beef and lamb contain higher levels of saturated fat than poultry and fish. Furthermore, high-temperature cooking (such as grilling, frying, and roasting) can significantly increase the formation of inflammatory AGEs. Highly processed foods also often contain high levels of salt, sugar, preservatives, and other additives that can cause adverse reactions in the body.
Therefore, for people with rheumatoid arthritis, the nutritional advice is to limit red meat consumption, and prioritize replacing it with healthier protein sources such as fish, poultry (skinless) and beans. At the same time, you should minimize canned and processed products such as sausages, bacon, and salami in your daily diet.
Mediterranean Diet: The optimal choice for people with rheumatoid arthritis
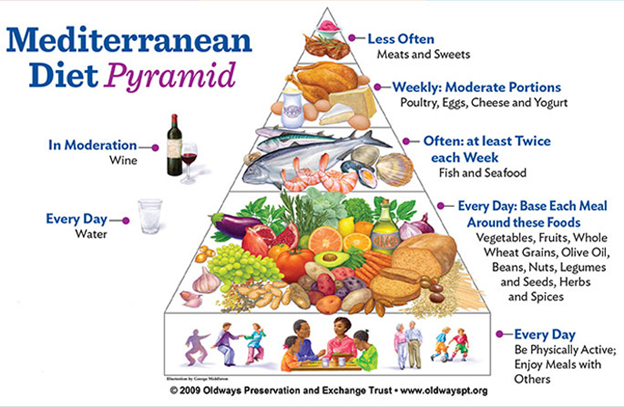
Keeping a list of foods to eat and foods to avoid can be complicated for people with rheumatoid arthritis. Instead, adopting a scientifically proven overall eating pattern is a simpler and more effective approach. Among them, the Mediterranean Diet stands out as the most ideal choice for rheumatoid arthritis patients.
Mediterranean diet improves rheumatoid arthritis
This diet is not a rigid menu but an eating pattern based on the traditional habits of people living in countries bordering the Mediterranean. Its advantages include:
- Plant-based: Increase green vegetables, fruits, whole grains, beans and nuts. These are rich sources of fiber, vitamins, minerals and thousands of antioxidants, anti-inflammatory (polyphenols).
- The main fat is extra virgin olive oil: Replace saturated fats with beneficial monounsaturated fats. Olive oil also contains the compound oleocanthal, which has anti-inflammatory effects similar to ibuprofen.
- The main source of protein is fish and seafood: Ensures a rich supply of Omega-3.
- Moderate consumption: Poultry, eggs and dairy products (mainly yogurt and cheese).
- Limit: Red meat, sweets and processed foods.
Basically, the Mediterranean diet is a perfect model since it is naturally rich in Omega-3, Vitamins, Calcium and healthy fats, while minimizing the inflammatory foods listed above.
However, in modern life, ensuring a perfect daily diet to provide enough specialized micronutrients such as calcium, vitamin K2, vitamin D3 or collagen Type II, glucosamine with effective doses can be a challenge, especially for the elderly or people with poor digestive absorption. This is when Medical Nutrition solutions are researched to have multi-target effects and promote their indispensable role.
As a result of cooperation between Nutricare and the Nutricare Medical Nutrition Institute – USA (NMNI-USA), Nutricare Bone is a scientific nutritional solution that improves the problems faced by rheumatoid arthritis patients through the following effective mechanisms:
- Impact on joint cartilage: To impact the joint cartilage structure that is being attacked by inflammation, Nutricare Bone provides glucosamine from the US that has been clinically proven to help joints become flexible and support joint pain relief.
- Strengthening bone foundation: Recognizing the risk of osteoporosis in rheumatoid arthritis patients, Nutricare Bone integrates the inseparable trio of calcium, vitamin D3 and vitamin K2. This combination supports optimal absorption of calcium and transport to the right location in the bone, allowing to strengthen bone density and reduce the risk of fractures.
- Protect and strengthen muscle mass: Nutricare Bone with a formula supplemented with vegetable protein and whey protein from the US participates in the protein synthesis process, supports the building and regeneration of muscle mass, and increases mobility. In addition, 50 nutrients with the Antioxidants system in milk support health and immune system enhancement, along with FOS fiber to support the digestive system for users.
Conclusion
Nutrition is a powerful tool for proactively managing rheumatoid arthritis. Instead of focusing on individual foods, aim for a holistic eating pattern, and the Mediterranean diet is the ideal choice. Remember that everyone has different needs. The most important step is to talk to your doctor to check your health indicators and get personalized nutrition advice, especially about adequate and proper nutrition. Combining smart eating with your doctor’s treatment plan is the most effective way to control your disease and live a healthier life.
References:
|
