 English
EnglishOsteoporosis prevention in the elderly: A Comprehensive guide to nutrition and lifestyle
Osteoporosis is a silent, progressive disease characterized by a decrease in bone density and quality, making them brittle and prone to fracture without obvious warning symptoms.
Osteoporosis prevention in the elderly
According to statistics from the Ho Chi Minh City Osteoporosis Association, an estimated 3.6 million Vietnamese people are facing osteoporosis and this number is expected to increase significantly. Millions of older people are facing the risk of serious fractures from even minor impacts in daily activities such as a slip or even a strong cough. A proactive prevention strategy, focusing on scientific nutrition and a healthy lifestyle is the key to preserving bone mass, maintaining flexibility and minimizing the risk of future fractures.
Correct understanding of the nature of osteoporosis
For effective prevention, we first need to understand the nature and mechanism of osteoporosis. Equipping ourselves with basic knowledge about the disease, risk factors and early warning signs allow us to have a comprehensive view and build an appropriate intervention plan.
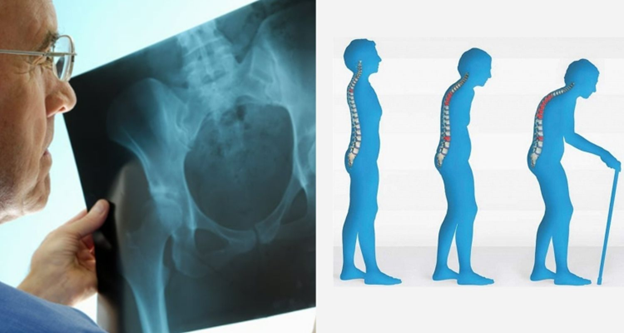
Osteoporosis – a dangerous health problem in the elderly
What is osteoporosis?
Osteoporosis is defined as a metabolic disorder of bone, which reduces bone strength due to a combination of two factors: reduced bone mass (or bone mineral density – BMD) and damage to the microstructure inside the bone. At that time, the bone becomes porous, thin, losing its ability to support and withstand force. The final and most dangerous consequence of osteoporosis is an increased risk of fracture. Typical fracture sites include the spine, wrist and especially femoral neck fracture. This is considered one of the serious events that can lead to disability, loss of mobility, expensive treatment costs and even increased mortality.
Top risk factors for osteoporosis in the elderly
Bone health is the result of a complex interaction between genetic factors and environmental and lifestyle habits. Identifying key risk factors is the first step in an effective prevention strategy. According to the International Osteoporosis Foundation (IOF), these factors can be classified into non-modifiable and modifiable groups. Here is a detailed analysis of the top risk factors.
- Age and natural aging process:
Our skeleton reaches peak mass around 25-30 years of age. After this stage, bone metabolism enters a state of natural imbalance. In which, the process of bone destruction (by osteoclasts) begins to occur faster than the process of new bone formation (by osteoblasts), leading to a decline in bone density and quality over time. - Gender and hormonal decline:
These two factors are closely related. Women are at significantly higher risk of osteoporosis than men for two main reasons. First, women tend to have smaller, thinner bones. Second, and more importantly, there is a sudden drop in estrogen levels during menopause. Estrogen acts as a powerful “protector” for bones, helping to slow bone loss. A sharp drop in estrogen levels leads to massive bone loss in the first few years after menopause. In men, the gradual decline in testosterone levels with age is also a factor in the loss of bone density. - Underlying medical conditions and medication use:
Bones are living organs and are directly affected by the overall health of the body. Several chronic diseases significantly increase the risk of secondary osteoporosis, including:
– Rheumatoid arthritis (RA): Chronic systemic inflammation can promote osteoclast activity.
– Other endocrine diseases: Hyperthyroidism, hyperparathyroidism, or diabetes.
– Gastrointestinal diseases: Malabsorption diseases such as Celiac or inflammatory bowel disease (IBD) interfere with the ability to absorb calcium and vitamin D.
– Chronic kidney disease: Affects vitamin D metabolism and mineral balance.
– In addition, long-term use of certain medications, especially corticosteroids (used to treat asthma and arthritis), is one of the leading causes of drug-induced osteoporosis.
- Chronic nutritional deficiencies:
This is a modifiable risk factor but has a huge impact. The process of maintaining bone structure and health depends directly on the supply of “it’s building materials” that includes:
○ Calcium and Vitamin D deficiency: This is the most common cause. Calcium is the main structural component, while Vitamin D is required for the body to absorb calcium from the intestine. Lack of either will disrupt the entire bone mineralization cycle.
○ Protein deficiency: A diet lacking in protein causes bones to lose their flexibility and become more fragile.
○ Severe malnutrition or underweight: Underweight (BMI below 19) is an independent risk factor, not only due to nutritional deficiencies but also due to reduced mechanical loading on the skeleton, which reduces osteogenic signaling.
Signs of early osteoporosis in the elderly

Bone pain is one of the early signs of osteoporosis
Osteoporosis often progresses silently, however, you can recognize the risk through some early clinical signs or slight changes in the body:
- Height loss: Loss of 2-4 cm or more in height compared to youth, often due to collapse of the vertebrae.
- Hunchback, postural changes: The upper back curves forward abnormally and the gait becomes more stooped. This is a result of weakened vertebrae.
- Dull bone pain: A feeling of pain along the long bones or in the lumbar spine, which increases with movement. The pain can be a sign of microfractures.
- Brittle, easily broken nails: Although not specific, this could be a sign that the body is lacking calcium and essential minerals for bones.
- Reduced grip strength: The ability to grip objects is significantly weakened. Many studies show that weak grip strength is associated with low bone density.
- Fracture after minor collision: This is the most obvious sign, as a minor fall can cause a fracture of the wrist, hip or spine.
Nutrition – a solid foundation for bone health
Osteoporosis can be prevented and its progression can be significantly slowed down. Nutrition plays a fundamental role in building and protecting the skeletal system from within.
Calcium: The main structural component of bones
About 99% of the body’s calcium is stored in bones and teeth, acting as the main mineral “material” to build and maintain bone density as well as determining the strength of the skeleton. The process of bone turnover where old bone is destroyed and new bone is created occurs continuously in the body. Providing enough calcium daily is a prerequisite for the bone formation process to take place effectively. According to the National Institute of Nutrition of Vietnam, the recommended calcium requirement for people over 50 years old is 1000 mg per day.
To achieve this goal, priority should be given to calcium-rich food sources such as milk and low-fat dairy products (yogurt, cheese); small fish that can be eaten with the bones (sardines, anchovies) along with dark green leafy vegetables such as bok choy, broccoli and beans, especially tofu.
Vitamin D: Essential nutrient for calcium absorption

Vitamin D stimulates calcium absorption from the intestine into the blood
Calcium supplementation is not optimal without vitamin D. Acting as a hormone, vitamin D plays a decisive role in increasing calcium absorption from the intestine into the blood. Its mechanism is to stimulate the synthesis of calbindin – a protein that transports calcium through the intestinal wall. Without enough vitamin D, the body can only absorb 10-15% of the calcium intake. Therefore, ensuring the recommended 800 – 1000 IU of vitamin D per day is extremely important. ⁵ The main source of supply is still through the synthesis process in the skin under the influence of sunlight. However, the elderly often have difficulty due to less outdoor activities and reduced skin synthesis ability. Therefore, it is necessary to proactively supplement from food sources such as fatty fish (salmon, herring), egg yolks and foods fortified with vitamin D such as milk and dairy products.
Protein: The collagen matrix of bone
If calcium is the building block of bones, then protein is the raw material that makes up the skeleton of bones. About 50% of bone volume and 1/3 of bone mass is made up of protein, mainly in the form of collagen matrix. This tough fibrous network creates a framework for calcium and other minerals to be deposited. A strong protein framework allows bones to increase their resistance to impact and reduce the risk of fracture.
Older adults need higher protein intakes to combat muscle loss (sarcopenia) and maintain bone health, with a recommended intake of 1.0–1.2g protein per kg body weight per day⁵. High-quality protein sources include lean meat, fish, eggs, dairy and legumes.
The role of other important micronutrients
In addition to the core trio of calcium – vitamin D – protein mentioned above, a healthy skeletal system also requires the synergy of many other micronutrients. Vitamin K, especially the form K2 (menaquinone), is needed to activate osteocalcin. This is a protein that “transports” and binds calcium to the skeleton, while also activating Matrix Gla Protein (MGP) to prevent calcium from being deposited in soft tissues and blood vessels.
Magnesium is also an important cofactor in calcium metabolism and is needed to activate vitamin D into its biologically active form. Meanwhile, zinc supports the activity of osteoblasts and the enzyme alkaline phosphatase, an important marker for bone mineralization.
Maintaining the health of the musculoskeletal system in the elderly requires a comprehensive nutritional solution that acts synchronously on the core components: bones – joints – muscles. Understanding this, Nutricare and the Nutricare Medical Nutrition Institute – USA (NMNI-USA) have successfully researched and developed the product Nutricare Bone with an optimal nutritional formula, supporting the improvement of bone and joint problems in the elderly.
Nutricare Bone helps strengthen bone structure through its exceptionally high calcium content (1800 mg/100g product). The effectiveness of calcium is optimized thanks to the smart “guiding” duo of vitamin D3, which stimulates absorption in the intestine, and vitamin K2, which plays a key role in directing calcium to attach accurately to the skeleton.
Along with strengthening bone density, the flexibility of joint cartilage is a key factor to ensure painless movement. Nutricare Bone is supplemented with glucosamine – a compound that has been clinically proven to reduce joint pain. Glucosamine participates in the process of increasing synovial fluid and cartilage cells, thereby allowing to lubricate and improve joint flexibility.
To improve the strength of the musculoskeletal system, healthy muscle mass acts as a support frame and a source of power for all movements, Nutricare Bone provides 50 nutrients with Whey protein from the US and easily absorbed vegetable protein. This protein ingredient provides essential amino acids, contributing to the synthesis and regeneration of muscles, thereby maintaining muscle strength and mobility.
Maintaining 2 glasses of Nutricare Bone every day not only helps improve osteoporosis but also strengthen the health of the musculoskeletal system, giving the elderly a full and active life.
Nutritional factors to be regulated for maintaining bone health

A high-salt diet increases the risk of calcium loss through urinary excretion
Building a strong skeletal system is not only about nutritional supplementation but also about controlling factors that may be harmful to the bones. Some components, when consumed in excess, can act as silent ‘enemies,’ weakening the bone foundation we are striving to build. Among them, the following four leading factors stand out:
- One of the leading risk factors is a diet rich in sodium (salt). High salt consumption significantly increases calcium excretion in the urine. This mechanism occurs in the kidneys, where sodium and calcium share the same reabsorption pathway. When sodium intake is high, the kidneys increase sodium excretion and inadvertently “pull” calcium along, forcing the body to mobilize bone reserves to maintain stable calcium levels in the blood.
- Similarly, excessive use of alcohol and beer also causes comprehensive negative effects on the skeletal system. Alcohol (ethanol) not only directly poisons bone-forming cells, reducing the ability to form new bones, but also disrupts hormones and hinders the intestinal absorption of essential nutrients such as calcium and vitamin D.
- In addition, the role of caffeine also needs to be considered carefully. Caffeine has a mild diuretic effect, increases a small amount of calcium excreted in the urine and hinders the absorption of calcium in the intestine. However, scientific evidence shows that this loss is not clinically significant if the diet ensures adequate calcium. The real risk only arises when high doses of caffeine (over 400mg/day) are consumed on a nutritional basis that is already deficient in calcium, causing even a small loss to not be compensated.
- Finally, carbonated drinks containing phosphoric acid are also a notable factor. Consuming large amounts of this acid can disrupt the balance between calcium and phosphorus in the blood. To adjust, the body will increase the secretion of parathyroid hormone (PTH), a hormone responsible for mobilizing calcium from the bones to put into the blood. Many studies have shown a link between daily consumption of carbonated drinks and reduced bone mineral density, especially in women.
Holistic lifestyle: a “shield” to protect the skeletal system
Nutrition is the foundation, but to make the “shield” to protect bones perfect, the role of exercise and scientific living habits is indispensable.
Increase physical activity

Greater physical activity supports the protection of strong bones
Wolff’s principle in bone biology states that bone remodels and strengthens itself in response to the forces applied to it. Mechanical stress from exercise stimulates osteoblasts to increase bone density and strength. A comprehensive exercise program should include:
- Weight-bearing exercises: This is the most important group of exercises for building bones, including brisk walking, stair climbing, and dancing.
- Resistance exercises: Lifting light weights, using resistance bands, and other exercises help increase muscle strength, thereby supporting and protecting bones better.
- Balance and flexibility exercises: Yoga and Tai Chi have been shown in numerous studies to improve balance, coordination, and significantly reduce the risk of falls in older adults.
Give up habits leaving bad impact on bones
Quitting harmful habits is an essential part of a bone-protecting strategy. Smoking has been shown to reduce blood flow to bones, inhibit the activity of bone-building cells, affect estrogen metabolism, and increase cortisol levels, a hormone that causes bone loss. At the same time, minimizing alcohol consumption is essential as it reduces calcium absorption and significantly increases the risk of falls and fractures.
Regular bone health screening
Regular screening plays an important role in the early detection of osteoporosis or osteopenia before complications occur. The common method today is to measure bone density by dual-energy X-ray absorptiometry (DXA Scan). The results are expressed as a T-score and osteoporosis is diagnosed when the T-score ≤ -2.5. International medical associations recommend postmenopausal women and men over 65 years of age as the main subjects for screening. However, people with other risk factors such as family history, long-term use of corticosteroids, or chronic diseases should discuss with their doctor to have appropriate screening indications.
Conclusion
The journey of preventing osteoporosis in older adults is a holistic investment, built on a sturdy three-legged foundation: smart nutrition – regular physical activity – and a scientific lifestyle. By prioritizing calcium-, vitamin D-, and protein-rich foods, combined with appropriate exercises, while also giving up harmful habits and proactively undergoing health screenings, you can keep your bones strong every day. See every meal as an opportunity to nourish your bones, and every step as an action to strengthen your health foundation. Don’t hesitate to consult with your doctor or a nutritionist to develop a personalized osteoporosis prevention plan that best fits your body condition and lifestyle.
References:
|
