 English
EnglishThe link between gut bacteria and diabetes
The intestinal microbiota, with trillions of microorganisms of hundreds of different species, plays a key role in digestion and immune regulation. Recent studies have shown that an imbalance in this microbiota is closely related to a number of diseases, including diabetes. So, is the intestinal microbiota really a “factor” in the pathogenesis of diabetes?
1. Gut microbiota and its function
In our intestines, there is an extremely rich ecosystem, called the gut microbiome. This ecosystem includes billions of microorganisms, such as bacteria, viruses, and fungi. Most of them live in the large intestine and play a very important role in health. Surprisingly, the number of bacteria in the body is even more than the number of human cells, research shows that there are about 40 trillion bacterial cells while there are only about 30 trillion human cells. The gut microbiome has about 1,000 different species of bacteria, each with its own task and most of them are extremely important to human health. They work together like an auxiliary organ, which can weigh up to 1-2 kg, almost the same weight as the brain. Although most gut microorganisms are beneficial, there are also some types that can cause disease.
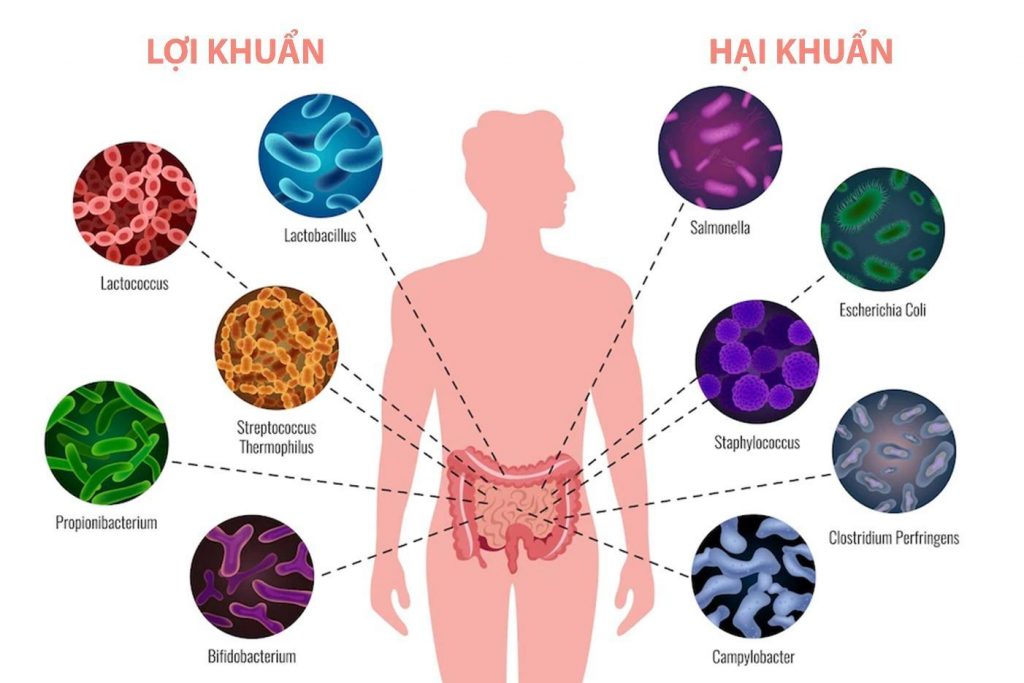
The intestinal microbiota is extremely rich and diverse
The gut microbiome has a profound effect on digestion. When the microbiome is disrupted, bacteria can overproduce gases and chemicals, causing unpleasant symptoms such as bloating and abdominal pain, which are common in people with IBS. In contrast, beneficial bacteria such as Lactobacilli and Bifidobacteria improve digestion by strengthening the intestinal barrier, preventing the invasion of pathogenic bacteria, and reducing the symptoms of irritable bowel syndrome (IBS). Supplementing with probiotics containing these beneficial bacteria can provide significant benefits for people with IBS.
The gut microbiome plays a key role in maintaining and strengthening the body’s immune system. Beneficial bacteria not only help control inflammation but also alleviate the symptoms of many different diseases. Specifically, they are able to reduce problems like antibiotic-associated diarrhea or Clostridioides difficile infection, constipation, inflammatory bowel disease (IBD), IBS, yeast infections, urinary tract infections, gum disease, lactose intolerance, eczema (atopic dermatitis), upper respiratory infections, and even sepsis, especially in infants.
Gut microbiota plays a key role in health
According to research by Bachelor of Nutrition Nguyen Thi Huyen – Department of Nutrition, 108 Central Military Hospital, bacteria in our digestive system have many positive roles on the body such as synthesizing essential nutrients, including vitamin K, vitamin B12, and biotin; supporting and strengthening the immune system; supporting the development of digestive health. Many studies show that the balance of bacteria in the intestines affects our health and susceptibility to certain diseases.
2. The link between gut microbiota and diabetes
The gut microbiome plays an important role in glucose and insulin metabolism – two key factors related to diabetes. Gut microorganisms have the ability to influence the body’s insulin sensitivity, that is, the ability of cells to respond to insulin to take up sugar from the blood. Some beneficial bacteria can produce metabolites that improve insulin sensitivity, while an imbalance in the microbiome can lead to insulin resistance.
In addition, the gut microbiome is also involved in blood sugar regulation. Some gut bacteria can produce short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate. These SCFAs have beneficial effects on glucose metabolism, enhancing insulin sensitivity and reducing inflammation. The diversity and balance of the gut microbiome may influence the risk of type 2 diabetes, and maintaining a healthy microbiome may be an important part of disease prevention and management. In this issue of Cell Metabolism, Krisko et al. (2020) demonstrate that the gut microbiome regulates glucose homeostasis through hepatic gluconeogenesis and not through thermogenic adipose tissue as previously believed.

Intestinal bacteria and diabetes are closely related.
A recent study of 33 infants at high genetic risk for type 1 diabetes found significant changes in the gut microbiota before the onset of the disease. Specifically, the diversity of the microbiota decreased dramatically, while the number of harmful microorganisms increased. This suggests that the gut microbiota may play an important role in the early development of type 1 diabetes. Furthermore, differences in the glycemic response of each person to the same food were also explained by differences in the activity of the gut microbiota.
Diabetes not only affects the body’s sugar metabolism but also significantly affects the gut microbiota. One of the most obvious effects is the change in the composition and biodiversity of the microbiota. This means that the number and type of bacteria in the gut can be altered, leading to an imbalance between beneficial and harmful bacteria. The causes of this change may stem from many factors, including unhealthy diet, the use of diabetes medications, and the chronic inflammation caused by the disease. Thus, it can be seen that diabetes and the gut microbiome have an interactive relationship, influencing each other and affecting the overall health of the patient.
3. Solution to improve intestinal health, prevent digestive complications in diabetics
Fiber plays a key role in maintaining intestinal health, especially important for people with diabetes. In particular, soluble fiber helps slow down the absorption of sugar into the blood, thereby controlling blood sugar more effectively; Insoluble fiber increases stool volume, promotes intestinal motility, and reduces constipation. To optimize the benefits, patients should increase the variety of fruits (such as apples, pears, oranges), green vegetables (broccoli, kale, carrots), and whole grains (oats, brown rice). Research shows that increasing fiber in the diet significantly improves blood sugar control, as fiber has a low glycemic index, increases blood sugar levels after meals slowly, thereby reducing the need for insulin production, allowing to protect pancreatic cells from deterioration.

Increase fiber in the diet of diabetic patients
Dividing your meals into several small meals a day to reduce pressure on the digestive system, especially the stomach. For people with diabetes, maintaining stable blood sugar levels is very important. By eating small and frequent meals. Dividing your meals into several small meals a day brings significant health benefits, especially for people with diabetes. First, this method helps reduce pressure on the digestive system, especially the stomach, making the digestion process easier. Second, and more importantly, eating small meals regularly enables stable blood sugar levels. When the body can absorb glucose more slowly and steadily, it avoids the condition of increased blood sugar after eating. This also helps control weight, an important factor in diabetes management. Experts recommend dividing into 5-6 small meals a day, instead of 3 large meals.
Saturated fats found in red meat, animal fats, and processed foods can increase bad cholesterol (LDL) and decrease good cholesterol (HDL), which is harmful to the heart, especially dangerous for people with diabetes who are already at high risk of heart disease. Instead, people with diabetes should prioritize healthy sources of unsaturated fats from fish (salmon, mackerel), nuts (almonds, walnuts), and beans. These fats not only provide energy but also support heart health, control blood sugar, and improve insulin sensitivity.

Foods containing healthy fats
In particular, the intestinal microflora plays an important role in maintaining overall health and controlling blood sugar. Probiotics found in unsweetened yogurt, kimchi, and other fermented foods provide beneficial bacteria, enabling intestinal microflora balance. Prebiotics found in onions, garlic, banana, and asparagus are a food source for probiotics, allowing them to grow and function more effectively. Supplementing probiotics and prebiotics helps improve insulin sensitivity, reduce inflammation, and enhance immune function. Many studies have shown that yogurt brings many health benefits to people with diabetes. Regular consumption of yogurt helps reduce insulin resistance, improve blood sugar control, reduce inflammation, and lower systolic blood pressure. Therefore, nutritionists encourage people with diabetes to add yogurt to their daily healthy diet. The Journal of Nutrition published a meta-analysis of 13 studies, showing that yogurt has benefits in reducing the risk of type 2 diabetes in healthy older adults.

Probiotic-rich foods are essential for diabetics
To maintain intestinal health and support diabetes control, it is extremely important to apply a scientific diet, a healthy lifestyle, and supplement probiotics. In particular, the product Glucare Gold with 100% soluble fiber FOS – prebiotic, which plays an important role as a food source for probiotics, is an ideal choice. FOS not only helps to regenerate beneficial bacteria but also minimizes common digestive problems such as constipation, indigestion, and bloating. Using Glucare Gold in combination with the above measures will significantly contribute to improving intestinal health and improving the quality of life for people with diabetes.
Conclusion: Through this article, we have clearly seen the close relationship between the intestinal microbiota and diabetes. A healthy intestinal microbiota plays an important role in maintaining blood sugar balance and preventing complications of diabetes. To improve intestinal health, we need to focus on a diet rich in fiber, limit sugar and bad fats, and maintain an active lifestyle. In addition, supplementing with probiotics is also a useful measure to increase the number and diversity of beneficial bacteria in the intestines. Taking care of the intestinal microbiota is an indispensable part of managing and preventing diabetes.
| References
2. https://benhvien108.vn/vi-khuan-duong-ruot-la-gi.htm 4. https://nhathuoclongchau.com.vn/bai-viet/tam-quan-trong-cua-chat-xo-trong-che-do-an-uong.html 5. https://www.vinmec.com/vie/bai-viet/bi-tieu-duong-co-duoc-sua-chua-khong-vi 6. https://www.nhs.uk/conditions/diabetes/ 7. https://www.healthline.com/nutrition/gut-microbiome-and-health |
