 English
EnglishEnd the anorexia obsession: Solutions from a balanced diet and lifestyle
Anorexia is a common problem that affects the physical, intellectual and psychological development of children. This article, from the perspective of a nutritionist, will provide a comprehensive solution, combining the establishment of a scientific schedule and a balanced diet, allowing parents to “rescue” their children from the obsession called anorexia.
Part 1: Understanding “anorexia” in children
Before finding a solution, parents need to clearly understand the nature of anorexia in their children.
What is anorexia? Common symptoms

Anorexia is a common nutritional problem that worries many parents
Anorexia is a condition in which a child refuses to eat, eats very little compared to the recommended needs according to age, holds food in the mouth for a long time without swallowing, only eats certain types of food or has negative behaviors during mealtimes (crying, vomiting…), or mealtimes last longer than 30 minutes.
Anorexia is divided into 2 common groups: physiological anorexia and pathological/psychological anorexia with the following differences.
- Physiological anorexia: Often occurs during certain stages of a child’s natural development such as when they learn to crawl, walk, teeth, or when there is a temporary change in appetite. This condition usually lasts a few days to a week and resolves itself when the cause is gone.
- ● Pathological/psychological anorexia: Longer lasting, may be due to underlying health problems (such as infections, digestive disorders) or psychological factors (stress, forced feeding). This case requires more intensive intervention to support the child to improve.
Prolonged anorexia leads to a number of serious consequences, including:
- Malnutrition, stunted growth, slow weight gain, slow height development: Lack of energy and essential nutrients hinders physical development.
- Weakened immune system: Children are more susceptible to infectious diseases asthey do not have enough micronutrients to build the body’s protective barrier.
- Mental retardation: Some important micronutrients for the brain such as iron, zinc, iodine, DHA are deficient and can affect the brain’s ability to learn and remember.
- Psychological impact: Children can become irritable, less flexible, and even fearful of mealtimes. Hence, the relationship between parents and children may also become more tense.
The underlying cause of anorexia in children
Identifying the correct cause is the first step to help parents solve their child’s anorexia problem, including 4 main groups of causes including:
- Anorexia due to psychology:
– Force feeding, scolding: Creating a stressful mealtime atmosphere can make children fearful and averse to food.
– Sudden change of environment: Going to daycare, moving house, having a new caregiver, etc. can also cause children to lose their appetite.
- Anorexia due to dietary mistake:

Improper nutrition is also the cause of anorexia in children
– Snacking too much, at the wrong time: Snacks that are too close to the main meal or contain a lot of sugar or fat make children feel full and no longer interested in the main meal.
– Monotonous, boring, unattractive menu: Repeating the same foods over and over again makes children lose interest and gradually causes them to lose their appetite.
– Processing is not suitable for age and chewing ability: Food that is too hard, too big or too soft can also make your baby uncomfortable.
– Let children watch TV/phone while eating: They are distracted, unable to focus on eating, unable to taste food, and unable to learn independent eating skills..
- Cause of irregular living habits:
– Irregular eating and sleeping hours: Children who do not have a fixed schedule disrupt their biological clock, affecting their hunger and ability to digest food.
– Lack of exercise: Lack of exercise reduces energy expenditure indirectly, making children not feel really hungry.
- Anorexia due to pathology:
– Infectious diseases: Sore throat, otitis media, respiratory infections, diarrhea… make children tired, uncomfortable and lose their appetite.
– Digestive disorders: Constipation, bloating, indigestion… also make children uncomfortable, reduce absorption and cause anorexia..
– Micronutrient deficiency: Lack of zinc, iron, selenium, B vitamins… can reduce appetite in children.
– Teething: Causes gum pain, discomfort when chewing and reduces children’s appetite, leading to temporary anorexia.
Part 2: The power of a scientific schedule in improving anorexia
A regular, scientific schedule plays a fundamental role in improving children’s anorexia.
Why a regular schedule is important?
– Stabilize biological clock: Allows the child’s body, including the digestive system, to function smoothly and the stomach secrete gastric juice more regularly at familiar meal times.
– Form conditioned reflexes with meals: When children get used to eating at fixed times, at that time their bodies automatically sends signals of hunger and want to eat.
Establish a schedule for your child
The schedule should be adjusted flexibly depending on the age and characteristics of each child. Below are some suggestions that parents can refer to:
- Mealtimes and snacks:
– Main meals (breakfast, lunch, dinner): Should be about 3 – 4 hours apart.
– Snack (mid-morning, mid-afternoon): At least 2-3 hours before main meals. Do not give snacks close to main meals (within 1-1.5 hours before main meals).
– Time of each meal: It should not last longer than 30 minutes. After 30 minutes, whether the child eats a little or a lot, end the meal.
- Bedtime:
– Make sure your child gets enough sleep according to their age (young children need 10-14 hours/day, including naps).
– Deep and on-time sleep helps children stay alert, feel comfortable and have a better appetite the next day.
- Time for exercise and entertainment:
– Encourage children to exercise at least 60 minutes a day through activities such as running, jumping, and playing outdoors,..
The “golden” rule for a daily schedule application

Persistence, listening and a happy mealtime atmosphere are the “golden” principles to enable good eating
- Persistence and consistency: This is the most important factor to improve anorexia in children. The whole family (including parents, grandparents, and caregivers) need to agree and follow the set schedule.
- Listen to your child’s body: While it’s important to maintain a regular schedule, parents should also be flexible in making adjustments based on their child’s cues (for example, if he/she seems more tired, you can put them to bed a little earlier). However, don’t completely break the structure of the schedule.
- Create a comfortable atmosphere, not rigid imposition: Parents need to remember that the goal is to create good habits, not to create more pressure for children.
Part 3: Balanced nutrition – The key to “opening” children’s taste buds
Along with a daily routine, a scientific and attractive nutritional regimen is the key factor to conquer a child’s difficult stomach.
Principles of menu creation for children with anorexia
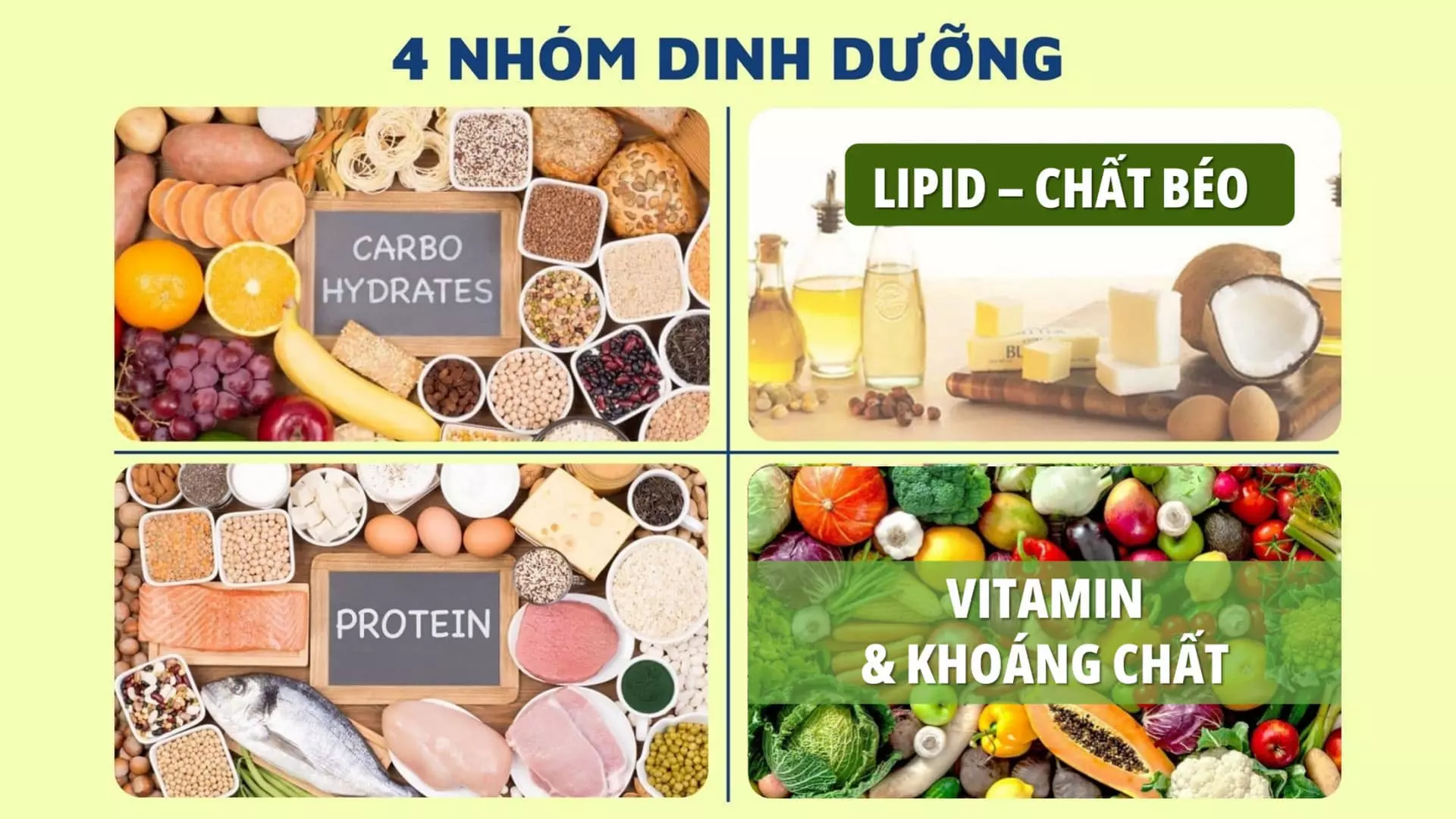
- Food diversification: Introduce slowly different types of food from the 4 main food groups. Don’t be discouraged if your child refuses the new food at first, be persistent and reintroduce it after a few days, it may take 10-15 tries for your child to accept it. At the same time, parents should change the way they cook regularly (boil, steam, stir-fry, fry, grill…) to create novelty.
- Balance nutrient groups:
– Protein: Protein diversity comes from foods such as meat, fish, eggs, milk, fish, shrimp and beans.
– Fat (Lipid): Fat is important for providing energy and absorbing fat-soluble vitamins (A, D, E, K). Parents should supplement fat from cooking oil, lard, butter, cheese and nuts for children.
– Starch (Carbohydrate): This is the nutritional group that provides energy for children’s metabolic and absorption activities. Carbohydrates usually come from rice, porridge, vermicelli, pho, bread or tubers.
– Vitamins and minerals: Pay special attention to the role of zinc, iron, lysine, and B vitamins in stimulating taste, enhancing metabolism, and absorbing nutrients. Green vegetables and ripe fruits are effective sources of these vitamins and minerals for children.
- Prioritize fresh, seasonal foods: Fresh, clean, seasonal foods often have delicious flavors, higher nutritional value, and ensure food safety, with the least amount of preservatives for children.
- Divide meals: If children eat less at each main meal, parents can increase the number of snacks but need to pay attention to ensure that the snacks are also nutritious enough to provide enough energy and nutrients for children during the day.
“The art” of preparing attractive dishes for children with poor appetite
Children are often attracted to things that are eye-catching and interesting. Therefore, preparing attractive dishes is also an effective solution for parents to improve the condition of anorexia in children.
- Eye-catching colors: Combine many colorful vegetables to make the dish look more attractive.
- Funny shape: Use food cutting molds to shape food (rice balls shaped like bears, rabbits; fried eggs shaped like flowers, etc.) to create attractive dishes that capture children’s imagination.
- Delicious flavor, suitable for children’s taste: Season moderately, not too spicy, too salty or too much strong spices. Prioritize the natural sweetness of vegetables and fish meat.
- Change the texture of the dish: From liquid (soup, porridge) to gradually thicker (mashed rice, minced meat), from soft (steamed fish) to slightly tougher (shredded chicken) depending on the age and chewing and swallowing ability of the child.
- Involve children in the preparation process (if possible): Let them pick vegetables, wash fruits or choose dishes allows them to be more excited about the meal they “contributed” to.
“Savior” food for children with poor appetite
Nutritious foods helps improve anorexia in children
- Taste stimulation group: Foods rich in zinc such as oysters, beef, chicken, foods rich in B vitamins such as whole grains, beans are proven to stimulate taste buds in children.
- Easily digestible and absorbable group: Porridge, soup, yogurt, and soft vegetables are a group of dishes and foods that are easy for children to digest and are more suitable for children in the stage of physiological anorexia such as teething, illness, and disease,..
- High energy group (if the child eats little): Butter, cheese or high-energy milk can be suitable solutions to compensate for the lack of energy in children’s diet. However, parents should not overuse them and need to balance and diversify with other foods to help children overcome anorexia.
To effectively solve the problem of anorexia and slow weight gain in children, parents can confidently choose Hanie Kid – a Medical Nutrition solution researched and developed by the Nutricare Medical Nutrition Institute – USA (NMNI-USA) and Nutricare specifically for children with anorexia and stunted growth. The highlight of Hanie Kid is the optimal nutritional formula, clinically proven to gain baby weight after 01 month of use. With the improved Pedia formula that meets the High Energy standard of 100 kcal as recommended by the World Health Organization WHO and high-quality protein, Hanie Kid allows children to gain healthy weight, quickly catching up with growth. In addition, the combination of lysine, zinc and B vitamins plays a key role in stimulating taste buds, helping children regain their natural appetite and improve anorexia. The trio of Calcium, Vitamin K2, D3 imported from the US provides and compensates for the lack of nutrients, thereby supporting height growth in children. At the same time, Hanie Kid is supplemented with 24-hour colostrum rich in IgG antibodies from the US combined with zinc and the Antioxidant system to increase your child resistance, HMO and soluble fiber FOS/Inulin not only support healthy digestion, prevent constipation but also enhance the ability to absorb maximum nutrients, creating a solid foundation for the comprehensive development of children. With these advantages, Hanie Kid is one of the nutritional solutions that effectively support parents on the journey to improve the health and stature of children.
Part 4: Standard dining table rules for mothers to create a disciplined environment for their children
Establishing consistent table manners helps children develop positive eating habits.
- Meal atmosphere is top priority: Parents should always keep the atmosphere happy and comfortable, avoid scolding, yelling, forcing or threatening children. At the same time, talk about happy topics, unrelated to children’s eating to avoid creating indirect pressure.
- Let your child feed himself (when possible): Respect your child’s autonomy, allowing them to decide what to eat first and how much to eat. Parents should encourage their children to feed themselves as soon as possible (around 1 year old or older) that allows them to feel more in control and interested.
- Do not use TV, phones, or toys to “entice” children to eat: These devices can easily distract children from chewing and tasting food. They also contribute to creating bad habits and make children only eat when they have these things.
- Praise and encourage children for their efforts: Even if your child only tries a small bite of a new food or eats a little better than yesterday, parents should acknowledge and praise their efforts.
- Parental persistence is the deciding factor: Changing a habit, especially an eating habit, takes a lot of time and patience. Therefore, parents should not give up too soon, but accompany and support their children on the journey to “cure” anorexia.
Part 5: Maintaining results and preventing anorexia from recurring
Once the child’s anorexia has improved, maintenance and prevention of recurrence are also extremely important.
Recognize early signs of anorexia in children

Recognizing the signs of anorexia returning helps parents find timely solutions to support their children
Parents should not be complacent even when their child is eating better. Watch for early signs that may indicate a return of anorexia:
- Children begin to be more picky, refusing more foods than before.
- Eating less significantly.
- Meal times lengthen.
- Interest in food decreases, children appear indifferent or irritable at mealtimes
Reinforce established healthy eating habits
When these signs of anorexia return, parents need to be more patient in reinforcing and maintaining previously established healthy eating habits. Some of the following points should be focused on:
- Continue to maintain a regular routine: Parents should remember that fixed meal times, bedtimes, and exercise times are still important foundations for improving anorexia in children.
- Be persistent in diversifying the menu and presenting attractive dishes: Be creative to keep meals fresh and vary the texture according to your child’s chewing ability.
- Always keep the meal atmosphere fun and positive: This is the key factor for children to love eating.
Flexible adjustment according to each stage of child development
- Children’s tastes and preferences may change over time: This is normal. Parents should observe and adjust the menu accordingly.
- As your child gets older, encourage them to be more involved in choosing and preparing food: Take them shopping with you, pick their own vegetables, or participate in simple cooking steps.
- Deal calmly with “crisis” periods: When children are teething, sick, or have major changes in their lives (going to school, moving house), they may lose their appetite again. At this time, parents need to be patient, understanding, and not pressure them, focusing on helping their children overcome that difficult period.
Conclusion

A balanced diet and routine are key to improve children’s appetite
Ending the obsession of anorexia in children is not an “impossible mission” if parents are equipped with the right knowledge and apply the right methods. The harmonious combination of a scientific, regular schedule and a balanced, diverse, and attractive diet is the golden key. More importantly, the perseverance, love, and understanding of parents are the key factors leading to success. Applying the above secrets not only allows your child to overcome the difficult stage of anorexia but also builds a solid foundation for healthy eating habits and comprehensive development of children in the future. Wishing parents success on their journey of raising your children.
References:
|
